Ayurvedic Treatment for Uveitis in Kerala
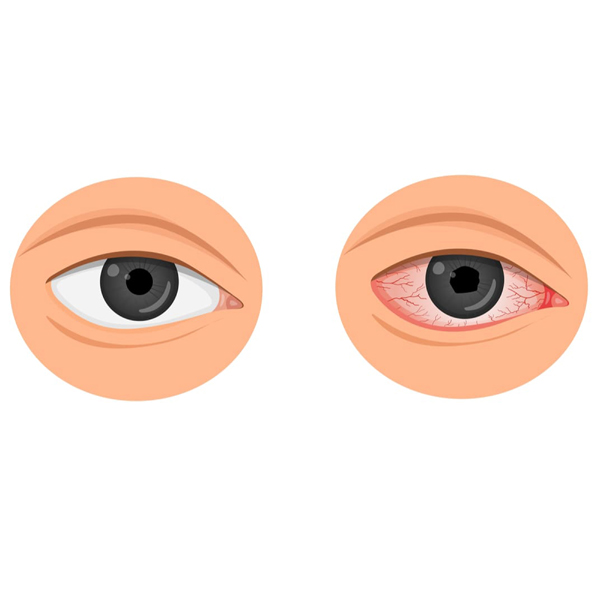
What is Uveitis?
Uveitis is the inflammation of the uvea, the middle layer of the eye, which includes the iris, ciliary body, and choroid. This condition can cause pain, redness, light sensitivity, and vision problems. Uveitis can affect one or both eyes and may lead to serious complications if not treated promptly. It can be acute, lasting a few weeks, or chronic, persisting for months or even years.
Symptoms
1. Eye Pain: Persistent pain or discomfort in the affected eye.
2. Redness: The eye may appear red or bloodshot due to inflammation.
3. Light Sensitivity: Increased sensitivity to light, causing discomfort or pain.
4. Blurred Vision: Vision may become blurry or distorted.
5. Floaters: Small spots or strings that seem to float in the field of vision.
6. Reduced Vision: A significant decrease in visual acuity.
7. Tearing: Excessive tearing or watery eyes.
8. Headache: Pain around the eyes that can radiate to the head.

Causes
Uveitis can result from various underlying causes, including:
1. Autoimmune Disorders: Conditions such as rheumatoid arthritis or lupus that cause the immune system to attack the eyes.
2. Infections: Bacterial, viral, or fungal infections that affect the uvea.
3. Trauma: Injury or trauma to the eye leading to inflammation.
4. Systemic Diseases: Conditions like sarcoidosis or Behçet’s disease that involve systemic inflammation.
5. Eye Disorders: Primary eye conditions such as retinal disease or eye cancer.
6. Unknown Causes: In some cases, the cause of uveitis may be idiopathic, meaning it is not clearly identified.
Types
Anterior Uveitis
Location: Affects the front part of the eye, including the iris and ciliary body.
Characteristics: Most common type, often presenting with redness, pain, and
sensitivity to light.
Intermediate Uveitis
Location: Affects the ciliary body and vitreous body in the middle of the eye.
Characteristics: May cause floaters and blurred vision.
Posterior Uveitis
Location: Affects the back part of the eye, including the choroid and retina.
Characteristics: Can lead to severe vision problems and is often associated
with systemic diseases.
Panuveitis
Location: Affects all layers of the uvea.
Characteristics: A more severe form involving widespread inflammation.
Diagnosis
Physical Examination: Includes checking for redness, pain, and visual symptoms.
Eye Examination: Using a slit lamp to assess inflammation and check the health of the uvea.
Fundoscopy: Examining the back of the eye to detect abnormalities in the retina and choroid.
Blood Tests: To identify underlying systemic conditions or infections.
Imaging Tests: OCT (Optical Coherence Tomography) or ultrasound to visualize internal eye structures.
Biopsy: In rare cases, a sample of eye tissue may be taken for analysis.
Treatment
Medications
Corticosteroids: To reduce inflammation and manage symptoms.
Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) to control inflammation.
Antibiotics or Antivirals: For infections causing uveitis.
Immunosuppressants: For autoimmune related uveitis.
Ayurvedic Management
Herbal Remedies: Using herbs such as Turmeric, Triphala, and Neem to reduce inflammation and support overall eye health.
Panchakarma Therapy: Detoxification treatments like Virechana (purgation) and Nasya (nasal administration of herbal oils) to balance doshas and eliminate toxins.
Diet and Lifestyle: Consuming cooling and anti-inflammatory foods such as
cucumber, mint, and coconut, and avoiding spicy or irritating foods.
Yoga and Meditation: Practices like Trataka (gazing at a fixed point) and Pranayama (breathing exercises) to enhance eye health and reduce stress.
Medical Procedures
Eye Drops: Used for localized treatment of inflammation and pain.
Injections: Corticosteroid injections may be administered directly into the eye.
Surgery: In severe cases, surgical interventions may be necessary to address complications.
Complications
Vision Loss: Severe inflammation can lead to permanent damage and loss of vision.
Glaucoma: Increased eye pressure resulting from uveitis can damage the optic nerve.
Cataracts: Clouding of the eye’s lens that may develop as a result of inflammation or corticosteroid use.
Retinal Detachment: Separation of the retina from the underlying layer due to inflammation.
Chronic Inflammation: Persistent inflammation that can lead to long-term eye
problems.
Prevention
- Regular Eye Exams: Early detection and treatment can prevent complications and manage symptoms effectively.
- Manage Systemic Conditions:Proper management of autoimmune or systemic diseases to reduce the risk of uveitis.
- Protect Eyes: Use protective eyewear to prevent trauma and reduce the risk of
infection. - Healthy Lifestyle: Maintain a balanced diet, avoid smoking, and manage stress to support overall eye health.
- Avoid Eye Irritants: Minimize exposure to substances or environments that can cause eye irritation.
FREQUENTLY ASKED
QUESTIONS
Can uveitis be fully cured?
Uveitis can often be managed effectively with treatment, but complete cure depends on the underlying cause and response to therapy. Timely and appropriate treatment is crucial to reduce inflammation and prevent complications.
Is uveitis contagious?
Uveitis itself is not contagious, but the underlying infections that can cause uveitis may be.
How long does it take for uveitis to improve with treatment?
The duration of improvement varies depending on the severity and underlying cause. Acute cases may improve within weeks, while chronic uveitis may require ongoing management.
Can Ayurveda help manage uveitis?
Ayurveda offers effective management of uveitis by reducing inflammation and balancing doshas. Ayurvedic treatments can complement conventional therapies and support overall eye health.
What should I do if symptoms of uveitis persist despite treatment?
If symptoms persist, it is important to consult with a healthcare provider for further evaluation and possible adjustment of the treatment plan. Regular monitoring and addressing any underlying conditions are essential.
Can diet affect uveitis?
Yes, a balanced Ayurvedic diet that includes anti-inflammatory and cooling foods can support eye health and potentially help manage symptoms of uveitis.
BOOK APPOINTMENT