Ayurvedic Treatment for Blepharitis in Kerala
What is Blepharitis?
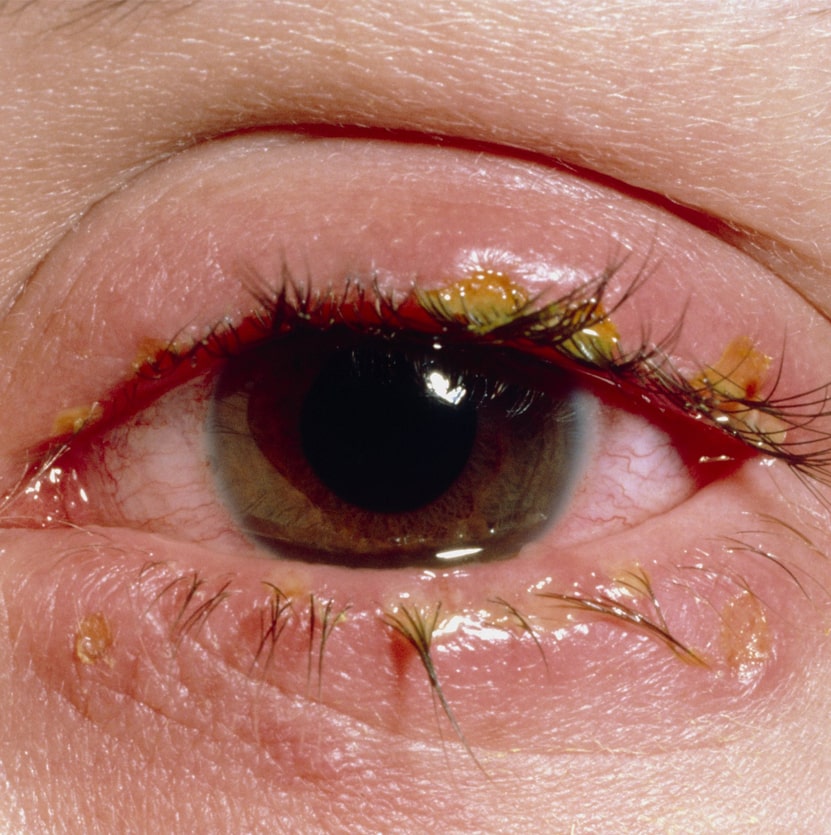
Blepharitis is an inflammation of the eyelids that affects the eyelashes or the edges of the
eyelids. This condition can cause redness, irritation, and the formation of crusts or scales on
the eyelashes. Blepharitis is a common, non-contagious eye condition that can be uncomfortable and persistent. It often occurs when the oil glands near the base of the eyelashes become clogged or irritated, leading to symptoms that can range from mild discomfort to more severe irritation and visual disturbances.
Symptoms
1. Red and Swollen Eyelids: Inflammation leads to redness and swelling of the eyelid margins.
2. Itching and Irritation: The eyelids may feel itchy or irritated, particularly along the lash line.
3. Crusting: Flakes or crusts form around the base of the eyelashes, especially upon waking.
4. Burning Sensation: A burning or stinging feeling in the eyes, often worsening in the morning.
5. Watery Eyes: The eyes may produce excess tears, leading to a watery appearance.
6. Dry Eyes: Paradoxically, blepharitis can also cause dry eye symptoms, with the eyes feeling gritty or dry.
7. Photophobia: Sensitivity to light, making it uncomfortable to be in bright environments.
8. Sticky Eyes: The eyelids may stick together, especially upon waking up in the morning.
9. Loss of Eyelashes: In severe cases, eyelashes may fall out or grow abnormally.

Causes
Blepharitis is often caused by a combination of factors that lead to clogged or malfunctioning oil glands at the base of the eyelashes:
1. Bacterial Infections: Overgrowth of bacteria, particularly Staphylococcus, on the eyelids.
2. Seborrheic Dermatitis: A skin condition that causes dandruff-like scales on the scalp and eyebrows, extending to the eyelids.
3. Rosacea: A skin disorder that causes facial redness and can affect the eyes and eyelids.
4. Meibomian Gland Dysfunction: Blocked or irritated oil glands along the eyelid margins.
5. Allergies: Allergic reactions to makeup, contact lenses, or environmental factors.
6. Mite Infestation: Microscopic Demodex mites that live in the hair follicles can contribute to blepharitis.
7. Poor Hygiene: Inadequate cleaning of the eyelids can lead to buildup of debris and oils.
8. Chronic Dry Eye: Reduced tear production or poor-quality tears can exacerbate blepharitis symptoms.
Types
Anterior Blepharitis:
Location: Affects the outside front edge of the eyelid, where the eyelashes attach.
Causes: Often associated with bacteria (e.g., Staphylococcus) or scalp dandruff.
Symptoms: Redness, itching, and crusting along the eyelid margins.
Posterior Blepharitis:
Location: Affects the inner edge of the eyelid, where it contacts the eyeball.
Causes: Often due to dysfunction of the Meibomian glands, which produce
the oily layer of the tear film.
Symptoms: Gritty or burning sensation, frothy or greasy tears, and crusting.
Mixed Blepharitis:
Characteristics: A combination of both anterior and posterior blepharitis symptoms.
Duration: Symptoms can be chronic and may require long-term management.
Diagnosis
Physical Examination: A thorough examination of the eyelids, lashes, and eye
surface using a slit lamp.
Swab Test: A sample of the discharge or crusts may be taken for laboratory analysis to identify bacterial or fungal infections.
Meibomian Gland Evaluation: Assessing the function of the oil-producing glands
along the eyelid margins.
Tear Film Test: Evaluating the quality and quantity of tears to rule out dry eye
syndrome.
Treatment
Lid Hygiene:
Warm Compresses: Applying warm compresses to the eyes to loosen crusts and open clogged oil glands.
Eyelid Scrubs: Cleaning the eyelid margins with a mild, non-irritating cleanser to remove debris and bacteria.
Artificial Tears: Lubricating eye drops to relieve dry eye symptoms associated with blepharitis.
Medications:
Topical Antibiotics: Antibiotic ointments or drops to treat bacterial infections.
Steroid Eye Drops: To reduce inflammation and irritation, often used for short periods.
Oral Antibiotics: In more severe or resistant cases, oral antibiotics may be
prescribed.
Lifestyle Modifications:
Avoid Makeup: Avoid using eye makeup until symptoms improve, as makeup can exacerbate the condition.
Manage Underlying Conditions: Treating associated skin conditions like rosacea or seborrheic dermatitis.
Maintain Good Hygiene: Regularly cleaning the face and hair, and avoiding touching the eyes with unclean hands.
Complications
Chronic Discomfort:
Persistent symptoms requiring ongoing management.
Corneal Damage:
Prolonged inflammation can lead to damage to the cornea, affecting vision.
Stye Formation:
Blocked oil glands can lead to painful lumps known as styes or chalazia.
Conjunctivitis:
Blepharitis can increase the risk of conjunctivitis, or pink eye.
Dry Eye Syndrome:
Ongoing inflammation can disrupt tear production and quality, leading to chronic dry eye.
Prevention
Regular Eyelid Hygiene:
Daily cleaning of the eyelids and eyelashes to prevent buildup of oils and debris.
Avoid Eye Irritants:
Using hypoallergenic and non-irritating makeup and skincare products.
Control Skin Conditions:
Managing underlying conditions like dandruff or rosacea that contribute to blepharitis.
Balanced Diet:
Consuming a diet rich in omega-3 fatty acids, which can help reduce inflammation and improve Meibomian gland function.
Frequent Hand Washing:
Keeping hands clean to avoid transferring bacteria or irritants to the eyes.
Ayurvedic Management:
Ayurveda treats blepharitis by balancing the doshas, particularly Pitta and Kapha, through therapies like seka, pratisarana, and the use of internal medicines. Key treatments include herbal eye drops with Triphala and Neem, Triphala eye washes, and the application of medicines to reduce inflammation. Additionally, a Pitta-pacifying diet, Nasya therapy, leech therapy and yoga practices like Palming and Trataka are recommended to support eye health and manage symptoms.
FREQUENTLY ASKED
QUESTIONS
Q: Can blepharitis be fully cured?
A: Blepharitis is a chronic condition that can be managed effectively with proper hygiene and treatment, but it may not be completely cured. Regular maintenance is key to keeping symptoms under control.
Q: Is blepharitis contagious?
A: No, blepharitis itself is not contagious, but the bacteria that contribute to it can be spread through poor hygiene.
Q: Can Ayurveda cure blepharitis?
A: Ayurveda can offer effective management for blepharitis by reducing inflammation, improving eye health, and addressing underlying imbalances, but ongoing care may be necessary.
Q: What home remedies can help with blepharitis?
A: Regular eyelid scrubs, warm compresses, and applying a natural eye wash like Triphala water can help manage symptoms.
Q: Can blepharitis lead to vision problems?
A: If left untreated, blepharitis can cause complications such as corneal damage, which can affect vision.
Q: Should I avoid using contact lenses with blepharitis?
A: Yes, it’s advisable to avoid contact lenses during flare-ups of blepharitis, as they can exacerbate irritation and discomfort.
Q: Can stress worsen blepharitis?
A: Yes, stress can exacerbate inflammatory conditions, including blepharitis, so stress management techniques like yoga and meditation can be beneficial.
BOOK APPOINTMENT